Understanding Autoimmune Diseases:
Causes, Triggers, and 10 Steps to Support Healing
Autoimmune diseases affect millions of people and are often misunderstood. Understanding the causes and triggers of autoimmune diseases is the first step toward finding effective healing strategies. Simply put, these conditions occur when your immune system, designed to protect your body from harmful invaders like viruses and bacteria, mistakenly attacks your healthy tissues. This immune dysfunction leads to chronic inflammation, pain, and various symptoms depending on the affected body part.
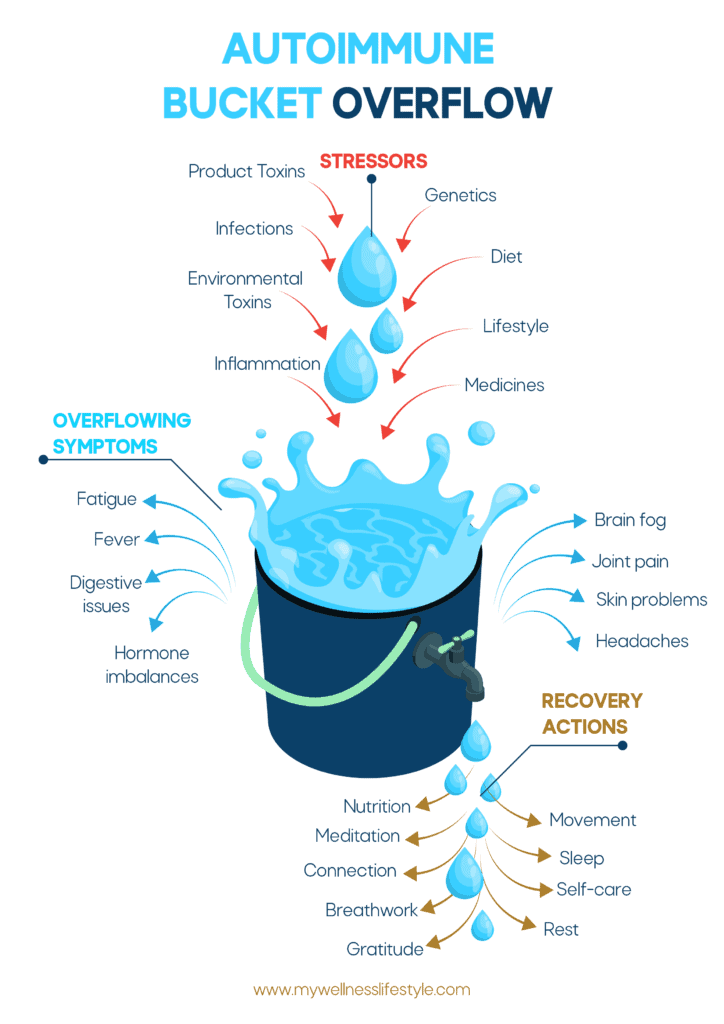
Think of your immune system as a bucket that collects stressors over time. Each potential trigger—like diet, chronic stress, environmental toxins, infections, or genetics—adds to this bucket’s capacity. As long as there’s room, the immune system can handle these stressors without symptoms. But when the bucket overflows, the immune system goes into overdrive, causing inflammation and multiple autoimmune symptoms. Healing often involves identifying and removing as many stressors and triggers as possible to bring the immune system back into balance.
Top Autoimmune Disease Triggers and How They Impact Your Health
Autoimmune disease is usually the result of multiple triggers acting together, not just a single cause.
Here are some common triggers:
- Diet: Certain foods can promote inflammation or disrupt gut health, which plays a critical role in immune balance. Gluten, sugar, and processed foods are particularly problematic for people with autoimmune conditions.
- Lifestyle Factors: Chronic stress, lack of sleep, and insufficient exercise weaken the immune system’s ability to regulate itself. Constant stress, especially, can put the body in “fight or flight” mode, which is taxing on the immune system.
- Environmental Toxins: Heavy metals, pesticides, and pollution accumulate in the body, increasing the burden on the immune system. Reducing exposure to these toxins in the food you eat, the water you drink and shower in, and the air you breathe, etc can relieve some of this load.
- Product Toxins: Everyday products like cosmetics, body wash, shampoo & conditioner, deodorants, household cleaners, and plastics contain chemicals that disrupt hormone and immune balance. For example, chemicals in plastics can leach into food and drink, adding to the body’s toxic load.
- Underlying Inflammation: Chronic inflammation caused by issues like leaky gut, mould exposure, heavy metals, gut imbalances, dental infections, and many more, makes the immune system hypersensitive and more likely to attack healthy tissues, leading to or worsening autoimmune diseases.
- Genetics: Some people are more prone to autoimmune conditions due to genetics. However, having a genetic predisposition doesn’t guarantee the disease will develop.
- Medicines: Certain medications, particularly antibiotics, hormonal contraceptives, and painkillers (NSAIDs), can disrupt the gut microbiome or increase inflammation, which may trigger autoimmune responses in susceptible people.
- Infections: Infections like Epstein-Barr virus (EBV), Helicobacter pylori (H. pylori), Strep throat, Lyme disease, Covid, or chronic bacterial imbalances can overstimulate the immune system, sometimes becoming the trigger that leads to the body attacking its own tissues.
How Autoimmune Diseases Progress and Why Triggers Matter
Autoimmune diseases typically progress through a combination of genetics and triggers, leading to a cycle of immune dysregulation and chronic inflammation.
Here’s how it often unfolds:
- Genetic Susceptibility: Some people inherit genes that make them more vulnerable to autoimmune conditions. However, these genes alone don’t cause the disease.
- Environmental or Lifestyle Trigger: An external trigger—such as a period of high stress, poor diet, infection, or toxin exposure—pushes the immune system into an overactive state.
- Immune Dysregulation: This immune activation can cause the immune system to lose its ability to distinguish between harmful invaders and the body’s own cells, leading it to attack healthy tissues.
- Chronic Inflammation: The continued immune attack causes chronic inflammation, which leads to the various symptoms of autoimmune disease, such as joint pain, fatigue, or organ damage.
- Increased Risk of Additional Autoimmune Diseases: Studies show that having one autoimmune disease increases the likelihood of developing more. Up to 25% of individuals with an autoimmune disease will develop a second one, within 3-10 years. Known as poly autoimmunity, this progression occurs when underlying inflammation and immune dysregulation remain unaddressed.
Common Types of Autoimmune Diseases
Autoimmune diseases can affect different parts of the body and show up as various conditions:
- Rheumatoid Arthritis (RA): The immune system attacks the joints, causing pain, stiffness, and possible joint damage.
- Hashimoto’s Thyroiditis: This condition targets the thyroid gland, often leading to hypothyroidism, with symptoms like fatigue, brain fog, and weight gain.
- Graves’ Disease: Causes the thyroid gland to become overactive, leading to symptoms like weight loss, anxiety, and tremors.
- Lupus (SLE): Affects multiple organs, including skin, joints, and kidneys, causing fatigue, joint pain, and rashes.
- Type 1 Diabetes: The immune system attacks insulin-producing cells in the pancreas, leading to blood sugar issues.
- Multiple Sclerosis (MS): Damages the protective covering of nerves, causing muscle weakness, vision problems, and coordination issues.
- Psoriasis: Causes rapid skin cell production, leading to red, scaly patches on the skin.
- Chronic Urticaria (Hives): Chronic hives have an autoimmune component, where the immune system attacks skin cells, causing persistent red, itchy welts on the skin.
- Celiac Disease: The immune system reacts to gluten, damaging the lining of the small intestine.
- Alopecia Areata: Attacks hair follicles, leading to hair loss in patches or across the body.
- Crohn’s Disease: Targets the digestive tract, leading to inflammation, abdominal pain, and digestive issues.
- Ulcerative Colitis: Causes inflammation in the colon, leading to abdominal pain and diarrhea.
- Sjögren’s Syndrome: Attacks glands that produce tears and saliva, causing dry eyes and mouth.
- Vitiligo: Destroys skin pigment cells, leading to white patches on the skin.
- Ankylosing Spondylitis: Targets the spine, causing pain and stiffness, especially in the lower back.
- Autoimmune Hepatitis: Attacks liver cells, leading to liver inflammation and potential liver damage.
- Myasthenia Gravis: Disrupts communication between nerves and muscles, causing muscle weakness.
- Addison’s Disease: Affects the adrenal glands, leading to fatigue, low blood pressure, and salt cravings.
- Pemphigus: Attacks the skin and mucous membranes, causing painful blisters.
- Dermatomyositis: Causes muscle weakness and skin rash, often affecting the arms and legs.
This isn’t the definitive list of autoimmune diseases; experts frequently identify between 80 and 100 confirmed autoimmune diseases and an additional 40+ conditions with suspected autoimmune components that are still under investigation.
10 Practical Steps to Healing Autoimmune Diseases Naturally
Healing from autoimmune diseases begins with reducing the stressors that fill your autoimmune “bucket” and implementing daily recovery actions to restore balance in your body. While healing is a gradual process, these practical steps can help reduce chronic inflammation, calm the immune system, and support your overall well-being:
- Nutrition: Focus on an anti-inflammatory diet rich in whole, nutrient-dense foods like vegetables, fruits, healthy fats, and lean proteins. Avoid common inflammatory triggers like gluten, dairy, processed foods, and added sugars. Eat Whole Real Foods!
- Hydration: Drinking plenty of clean, filtered water daily helps to flush toxins, reduce inflammation, and support immune function. Start your day with a glass of water with a pinch of Celtic salt to enhance mineral balance, rehydrate and improve energy and digestion.
- Movement: Engage in gentle, regular exercise like yoga, qi gong, walking, or swimming. These low-impact activities improve circulation, reduce stiffness, and support overall physical health without overtaxing the body.
- Sleep: Prioritize restorative sleep by creating a consistent sleep schedule and a calming bedtime routine. Sleep is essential for repairing the body, regulating inflammation, and improving energy levels.
- Sunlight and Nature Exposure: Spend time outdoors daily to soak up natural sunlight, which helps regulate your circadian rhythm, boosts Vitamin D levels, and reduces inflammation. Connecting with nature can also lower stress and promote a sense of well-being.
- Self-Care and Rest: Schedule time for self-care activities like baths, reading, or quiet time. Balancing activity with intentional rest helps the body recover and lowers overall stress levels.
- Meditation: Incorporate mindfulness or meditation practices into your routine to reduce stress, which is a major contributor to autoimmune flare-ups. Even 5-10 minutes a day can promote a calmer nervous system and better immune regulation.
- Connection: Build and maintain strong relationships with family, friends, or support groups. Emotional connection can reduce feelings of isolation, improve mental health, and indirectly support physical healing.
- Breathwork: Practice deep breathing exercises to calm the nervous system and lower stress hormones. Techniques like diaphragmatic breathing or box breathing can promote relaxation and reduce inflammation.
- Gratitude: Foster a positive mindset by practicing gratitude daily. Reflecting on things you’re thankful for can reduce stress, improve mood, and help shift focus toward healing.
By consistently integrating these steps into your lifestyle, you can reduce the overflow of stressors in your autoimmune “bucket” and support your body’s natural healing processes. Healing is not an overnight process, but small, daily actions can lead to meaningful progress over time.
Why There’s No “One-Size-Fits-All” Approach
Because autoimmune diseases are triggered by a variety of factors, no single treatment works for everyone. Experts like Dr. Mark Hyman and Dr. Libby Weaver emphasize that each person’s condition is unique, and an effective approach considers the root causes specific to the individual. Healing will require a blend of dietary changes, lifestyle adjustments, stress management, and detoxification to bring the immune system back into balance.
Autoimmune diseases are challenging, but understanding how they work can empower us to make choices that reduce inflammation, support immune function, and manage symptoms. Taking small steps like improving diet, reducing toxin exposure, and managing stress can make a difference over time and lead to a better wellness lifestyle.
This overview gives a foundational understanding of autoimmune diseases, helping readers recognize how diet, lifestyle, and the environment all play roles in your health. By learning about the common types, causes, and triggers, readers can begin to take proactive steps on their journey to wellness.